We try to simulate a patient with a spleen rupture after a bike crash. Currently I just trigger a internal spleen rupture with severity 1 but the patient doesn’t really get unstable. Over a timeframe of ~30min the heartrate goes from 73 to 125 and blood pressure falls from 114/73 to 87/68. After 30mins the patient seems to stabilize and his vital parameter don’t get any worse. For our application he should worsen much quicker. Blood pressure should fall to 60/40 in a few minutes and he should go into cardiac arrest after around 15min. Any tips on how to approach this? I also tried to trigger multiple hemorrhages to speed things up but that just crashes the Pulse Engine after some time.
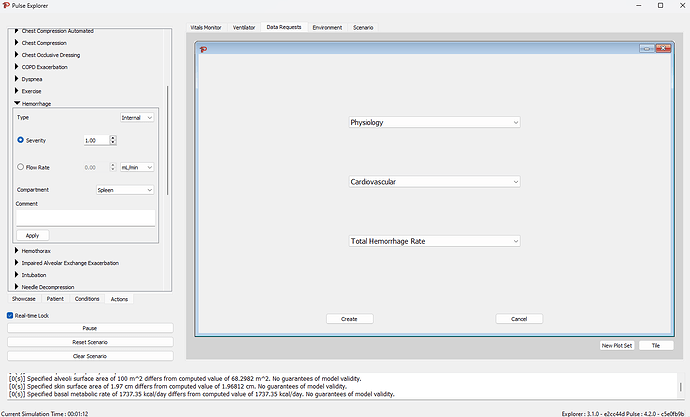
You can setup a data request to view the hemorrhage rate of all the blood loss in the explorer like this:
Applying that hemorrhage gives a flow rate in mL/s (I need to update the Explorer to display the units)
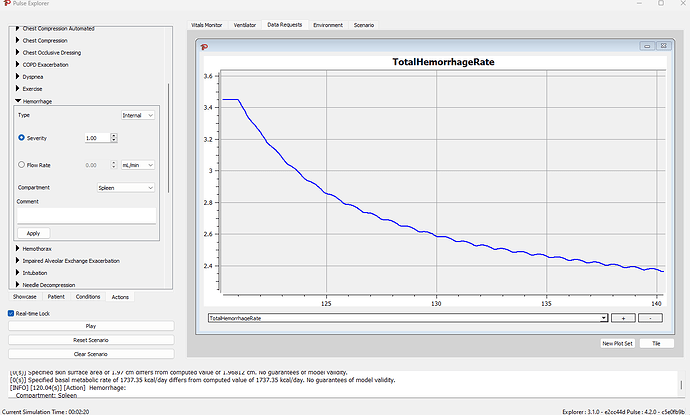
So this bleed starts off around 3.5 mL/s, and drops with the pressure at the spleen.
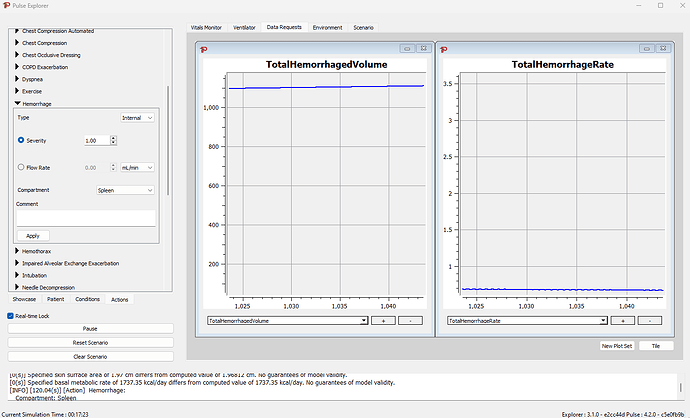
You can also view the total volume lost (in mL) the same way by either clicking the + button or adding a new plot set (which allows you to view both graphs at the same time)
After about 15m the system has lost about 1 L of blood, and the flow has stabilized
I assume this is due to the internal cavity being filled to its maximum compliance with blood and this results in the patient ‘stabilizing’ as the blood does not have anywhere else to go in our model.
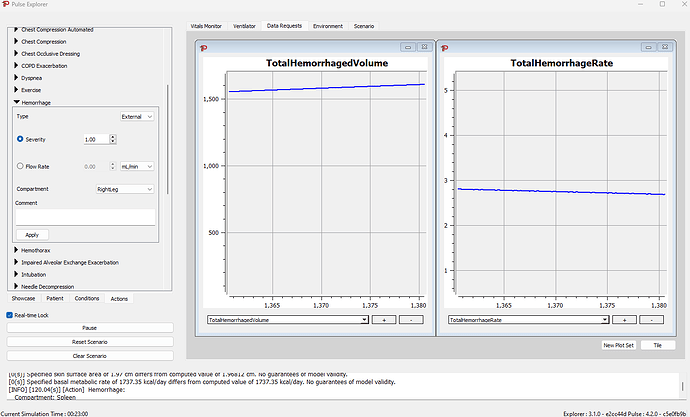
You could change the hemorrhage type after 20 min to an external hemorrhage, representing opening up the abdominal cavity, and releasing the blood to flow out of the body. This will result in increasing the flow and blood loss now that the blood has somewhere to go.
@rachel.clipp can you provide some more detail on our internal hemorrhage model in this reguard?
Hello,
I definitely agree that our internal hemorrhage model is not supporting enough volume loss and then almost seals the wound with the pressure. This is something we need to look into correcting. However, a full rupture of the spleen is probably not represented well by a hemorrhage even at severity 1. I would imagine you would also get venous loss and would need at a minimum a hemorrhage on both the arterial (spleen) and venous (vena cava) side. However, the pain and trauma of rupture would also probably lead to shock or other symptoms that are not well represented by simply the hemorrhage.
A pressure drop as quickly as you are suggesting would be a massive hemorrhage that is 40% of blood loss in a few minutes if just hemorrhage alone. Spleen blood flow is not that high, so the arterial blood flow cannot account for that.
Thanks,
Rachel
Thanks for the fast response!
Maybe I should add here that the goal of our application is not to super accurately simulate a spleen rupture but more about diagnosing an internal bleeding and taking the right actions to stabilize the patient.
Patient should:
- In the beginning HeartRate and RespiratoryRate go up and BloodPressure starts to go down
- After enough blood is lost (~10min) the patient gets unconscious which leads to very low RR (< 6)
- After ~15min most parameters should get very low and the patient dies due to oxygen and blood loss.
- When treated with intubation and volume therapy the patient should stabilize slightly
Things I tried:
- Trigger stronger hemorrhages (An external vena cava hemorrhage helped a lot with getting the patient unstable)
- “Acute stress” got the HR up a little.
What other actions/settings/features inside the PulseEngine could I generally use to simulate the course of a spleen rupture and the trauma/shock caused by it? (I currently struggle most the with point of unconsciousness and the RR going up and down)
I also have the issue that the PulseEngine crashes due to the hemorrhage when the patient gets too low:
[ERROR] [68.36(s)] Can’t transport with a negative volume included. Node = RightPulmonaryVeins. Volume = -0.155723 mL
Is there something I can do about that?
The negative volume means you have bleed out soo much blood that our maths broke.
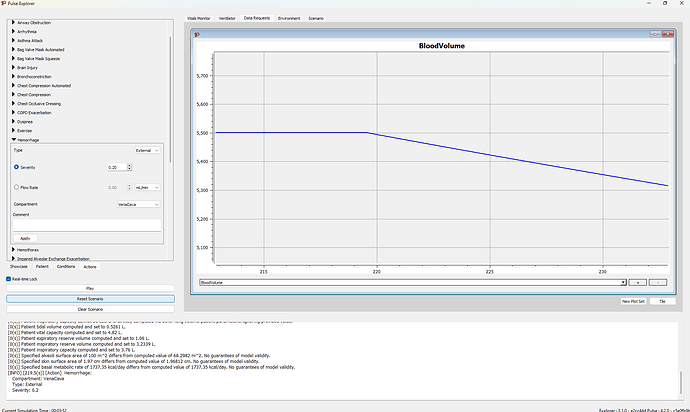
So the first thing I would do, is create a data request to view the blood volume an an External Vena Cava hemorrhage of 0.2 severity
We are starting with 5.5L of blood, so I targeted a 25% loss of blood since a loss of more than 35% is considered hypovolemic shock… so get the blood volume down to ~ 4L and then turn off the vena cava hemorrhage (Set severity to 0) (This took about 6 min of simulation time). Then apply the Spleen Internal hemorrhage. I tried a severity of 1.0, and that got the BP way to low… like 45/33… So maybe go for a 15-20% initial blood loss…
Again, watch that blood volume, you really should not simulate a quick loss > 35-40% or our simulator will run out of blood in places
I agree that the patient gets unconscious which leads to very low RR (< 6) is the tricky part… let us think on that a bit…
Hello,
We actually have a issue in our backlog because the respiration rate is too low. The literature generally supports a respiration increase to 24-30 or higher for significant blood loss. We have been working to improve the model for this. We have not considered a drop in respiration at this point. Do you have more information you could provide on why this would happen?
Thanks,
Rachel
I now trigger a vena cava external for about a minute and then switch to the spleen internal. I then use “acute stress” and “dyspnea” to get the HR and RR up. That should do the job for our application but needs more testing.
I totally agree with you that the respiratory rate should go up when the body suffers from significant blood loss and the engine doesn’t really do that at the moment. That’s why I tried to work with stress and dyspnea there. But at some point the blood loss is so significant that the body shuts completely down. I will simulate that part with a cardiac arrest for now. But I have no medical background so I forwarded your question to our team:
"In the event of severe blood loss, an attempt is made to compensate for this by breathing faster, by which time the patient is already in shock.
In the event of life-threatening blood loss, the patient becomes unconscious, due to the fact that there is already SO little blood and therefore oxygen in the body that the brain is no longer sufficiently supplied, the patient loses consciousness. At the same time, the brain no longer controls the vital functions properly (due to a lack of oxygen, resulting in reduced respiratory drive) and the organs are extremely undersupplied with oxygen, which also means that the lungs themselves no longer function properly. Above all, breathing becomes irregular and decreases overall in frequency (but it is not the case that they simply breathe slower and slower in a relaxed manner… but sometimes they breathe three times quickly in succession, then not at all for 10 seconds, then again, then not for a few seconds and the total breaths decrease per minute until the patient would no longer breathe)
In short: In the event of blood loss, the respiratory rate first increases to compensate for the lack of oxygen, but if the bleeding or lack of oxygen is extreme and cannot be compensated for, breathing no longer functions normally (i.e. breathing becomes very irregular and decreases in frequency)."
(Translated with DeepL)
Thanks for that information.
We are attempting to model the compensatory phases of hemorrhage loss. So we are expecting an increase in respiration rate in response to the low SPO2, as you know that is not happening. It is on our list to fix.
We produce an event when cardiovascular collapse is reached, around 40 mmHg. This seems like perhaps the appropriate place to use cardiac arrest? Cardiac arrest is what I would recommend there, as well.
Thanks,
Rachel